Before continuing with the blogs about the PCC I wanted to address a question that was presented to me: since Debra has stated that they would post the videos of the conference on their website, why bother doing the blog?
Aside the fact that I would have rather been ‘thanked’ than made me wonder if I am wasting my time, we do not know if Debra will post these videos next week or next year. But even if it’s next week, I also believe that the more ways this information is available the better, and this is what this website is about, INFO. But that’s just my opinion, take it or leave it.
Ok, now, let’s continue. The talks that followed which I will talk about today were about Prenatal Diagnosis of EB and Surgical Management of EB.
Prenatal Diagnosis of Epidermolysis Bullosa
This talk was presented by Dr. Sharon Glick and not surprisingly, I unfortunately did not take any notes, nor took photos of the slides. My apologies. I guess I thought this talk did not apply to me because I am a little too old to be having more children, and I did not learn anything new as well. If there was something new, I wrote it down. HOWEVER, here’s some links to know more about it and my summary of what I know about this topic.
http://www.debra.org/abouteb#prenatal
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2230038/
Basically there is no test to find out if you’re a carrier of EB (for Recessive forms of EB) prior of your child being born with EB. I get this question ALL THE TIME so I want to make sure I reiterate this point. I was told by various doctors that it would be like looking for a needle in a haystack. Of course for the Dominant forms of EB it’s evident since one of the parents has the condition. Of course there is always that spontaneous mutation which is not inherited, but, I digress. Determining the type of EB in a particular family member can be achieved through studies of a skin biopsy taken from the affected family member. The skin sample is then sent to a laboratory to confirm the subtype and the DNA mutation(s). This process may take several months, so they always suggest to do this BEFORE trying to get pregnant again. When a pregnancy occurs, DNA taken from the fetus can be studied for the presence of these mutations through CVS or amniocentesis. Preimplantation Genetic Diagnosis (PGD) is done prior to pregnancy, and improves the chances of having an EB free child. PGD is accomplished with in-vitro fertilization.
I wish I knew where to send parents for this PGD, I know of one clinic in New Jersey that does it (New Jersey Fertility Center) but not sure of others. I would suggest to contact the Debra Nurse, she is a wealth of information! If you know of a clinic that helps EB parents with PGD, please leave a comment below. THANK YOU!
Now… here’s a little about MY particular situation, maybe someone can relate or this info can perhaps help. When Nicky was 9 months old (in the summer of 1997) Stanford took blood samples from him, myself and his dad to find out the genetic mutation. All of that came back inconclusive, Dr. McGuire wrote me a handwritten letter (which I still have, I can’t believe he actually hand wrote a letter just to me!) apologizing and said to try to re-do the test at a later date when technology improved. I was never aware technology improved until THIS PCC. That’s how out of it I have been! I was sitting next to Geri, the Debra Nurse, and she told me to do it now. Of course I would not be doing it for future children of mine but I am curious to find out if my Connor is a carrier or my niece Paola is a carrier. I have other nieces/nephews as well and if I can avoid another RDEB family member and all the pain and suffering associated with it, I will gladly do it. The problem is that I do not know if the insurance will pay for it this time, but maybe they will since the first time it didn’t work? I will certainly try to get a referral.
GeneDx (www.genedx.com) is currently performing genetic analysis for the most common known mutations of many of the forms of EB but it’s pricey, as I am told (around $6,000) and it’s hard to get the insurances to pay for it. Stanford is also doing a Characteristic Study for those that could travel there, and it’s free.
If anyone has anymore important info about this subject, please leave a comment below. THANK YOU!
Here is the video of this presentation, courtesy of Debra:
DNA Q&A Video:
Surgical Management of Epidermolysis Bullosa
 Dr. Peter J. Stern did this talk about Hand surgeries for patients with RDEB. A lot of the slides were VERY graphic so I did not take photos of those-they were just hard to watch, even for me who has seen it with my own two eyes. Sigh.
Dr. Peter J. Stern did this talk about Hand surgeries for patients with RDEB. A lot of the slides were VERY graphic so I did not take photos of those-they were just hard to watch, even for me who has seen it with my own two eyes. Sigh.
First he went through the terminology, which includes words such as “non-pliable skin”, “pseudosyndactyly”, “thumb adduction”, “digital flexion contractures”, “acral osteolysys”, this last one meaning the dissolution of bone/nails.
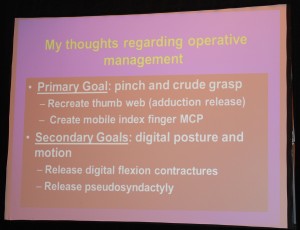
He states, like the slide explains, that his Primary Goal with hand surgeries, depending on the level of deformity, is to make sure the patient can pinch and grasp things. Being able to pick up a pen and write for example, is a big issue. His secondary goals include releasing pseudosyndactyly to get the fingers in a more straight or at least curved mode rather than a fist so they may have some use of it.
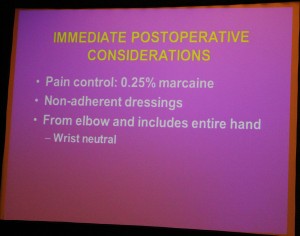 He stated that he uses skin grafts for his hand surgeries, taken from another part of the body, and talked about the importance of pain medication and wound dressing/splints etcetera, making sure the wrist can rest in a neutral mode.
He stated that he uses skin grafts for his hand surgeries, taken from another part of the body, and talked about the importance of pain medication and wound dressing/splints etcetera, making sure the wrist can rest in a neutral mode.
Now, here’s my 2c for whatever they are worth and what has worked for my son and my observations… this may or may not be what works for other RDEB patients, but it is what has worked for Nicky:
The first thing I wished I had known when Nicky was little was that the hand was not only going to web/mitten from wounds healing wrong, but ALSO from the thick scaly skin that eventually would become so tough that it would close the hand in a cocoon. This is why, in my view, Nicky’s hands mitten so fast without bandaging, the thick scaly skin does not grow and gets tougher by the day.
The bandaging instructions-complete with videos- are linked below, but I do something more to prevent the skin to get tougher which for my son is KEY: I wrap each finger with Vaseline Gauze, which lately I coat with various oils that soften the skin even more, such as Coconut Oil, Vitamin E, and I am now trying this Argan Oil, all soften the skin even more. I also SOAK his hand in these oils before rewrapping them. My goal for Nicky is to make these hand surgeries as RARE as possible by preventing the skin to get that bad to begin with. My post with post-surgery pics from earlier this year is here. Note that I was able to prevent a repeat surgery on that hand for 12 years while keeping the mobility of the hand this way, and Nicky would not have it any other way.
Dr. Ladd from Stanford, which is Nicky’s hand surgeon, does not uses skin grafts, but does uses the pins like Dr. Stern showed, and a cast. She cast the hand in a splint, well bandaged, and takes it off 2 weeks later. We were very happy with the results, but knew first-hand that it would take at least 6-8 weeks for the hand to completely heal and that we had to make sure to wrap it with the appropriate tension to keep the improvements achieved by the surgery. 8 weeks later we started the weekly physical therapy and Nicky uses a nightly splint to keep the thumb out and the palm open. He is so happy with the surgery that he now wants to do the other hand, which was operated on 10 years ago. The only problem with that hand is that the pinky has now ‘disappeared’ in the hand and the thumb is almost unusable due to the webbing. The other 3 fingers though are GREAT! All thanks to the wrapping, no doubt. Now with the addition of the oils and splints I know I can make a big difference and keep the hands from webbing even longer.
Here is the video of this presentation, courtesy of Debra:
Here’s the presentation about hand surgeries done at the 2010 Conference:






